Author: Fernanda H. P. de Moraes, Kangjoo Lee, and Julia W. Y. Kam |
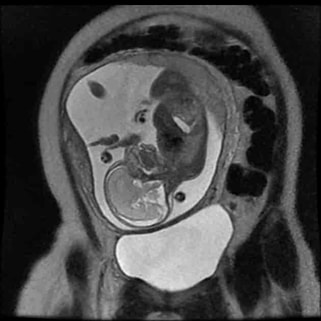
| The primary mission of the OHBM Women Faculty Special Interest Group (WF-SIG) is to help women principal investigators (PIs) connect and network with each other. Peer-to-peer networking is an effective, low-cost intervention that encourages female neuroscientists to collaborate in cross-disciplinary teams and overcome gender-related challenges (1). Our official in-person launch event at this year's annual OHBM meeting marks the first step towards connecting and empowering women-led research teams in the neuroimaging community. Logo Design: Jingyuan Chen, Arts Officer At the launch event, we unveiled the new logo that was crafted for the OHBM Women Faculty SIG by our Arts Officer, Dr. Jingyuan Chen (Assistant Professor, Martinos Center for Biomedical Imaging). |
Naomi Gaggi
Scientific writing workshop by Bradley Voytek, hosted by the SP-SIG
Communications Committee Lay Media team
Invitation to public events on brain imaging science (English and French language)
More details are provided below. You are invited to attend and to share this invitation with anyone who might be interested in this event.
Place: Grande Bibliothèque (475 Boul. de Maisonneuve E, Montréal, at Berri-UQAM metro station)
Date: Tuesday July 18, 2023
Time (talks in French): 6:00 pm (doors open at 5:30 pm)
Time (talks in English): 8:00 pm (doors open at 7:30 pm)
Tickets: free, but limited numbers available! Register quickly using the link below.
Register for French lectures: imagerieducerveau.eventbrite.ca
Register for English lectures: brainimaging.eventbrite.ca
Talks are aimed at the general public, and for each language session, there will be three talks of around 20 minutes, along with a Q&A session after.
Talks in English will be given by:
Dr. Alan Evans (A hitch-hiker's guide to mapping the brain)
Dr. Emily Coffey (Altering sleep and memory with sound)
Dr. Robert Zatorre (The neuroscience of music and why we love it)
Talks in French will be given by:
Dr. Sylvain Baillet (Tempête dans la boîte crânienne !)
Dr. Delphine Raucher-Chéné (Apports de la neuroimagerie en psychiatrie : en quoi étudier le cerveau nous aide à mieux comprendre les problèmes de santé mentale ?)
Dr. Anne Gallagher (Toute la lumière sur le développement du cerveau)
Le mardi 18 juillet, des neuroscientifiques d'universités québécoises présenteront les recherches liées au fascinant domaine de l'imagerie du cerveau. Les conférences seront données en anglais et en français, et sont gratuites pour le grand public.
Plus de détails sont fournis ci-dessous et dans les affiches ci-jointes. Vous êtes invités à y assister et à partager cette invitation avec toute personne susceptible d'être intéressée par cet événement.
Place : Grande Bibliothèque (475 Boul. de Maisonneuve E, Montréal, à la station de métro Berri-UQAM)
Date de l'événement : mardi 18 juillet 2023
Heure (conférences en français) : 18h00 (ouverture des portes à 17h30)
Heure (conférences en anglais) : 20h00 (ouverture des portes à 19h30)
Billets : gratuits, mais en nombre limité ! Enregistrez-vous rapidement en utilisant le site ci-dessous.
Billets pour les conférences en français : imagerieducerveau.eventbrite.ca
Billets pour les conférences en anglais : brainimaging.eventbrite.ca
Les conférences s'adressent au grand public et chaque session linguistique comprendra trois conférences d'environ 20 minutes, suivies d'une séance de questions-réponses.
Les conférences en français seront données par :
Dr. Sylvain Baillet ( Tempête dans la boîte crânienne ! )
Dre. Delphine Raucher-Chéné ( Apports de la neuroimagerie en psychiatrie : en quoi étudier le cerveau nous aide à mieux comprendre les problèmes de santé mentale ? )
Dre. Anne Gallagher ( Toute la lumière sur le développement du cerveau )
Les conférences en anglais seront données par :
Dr. Alan Evans ( A hitch-hiker's guide to mapping the brain )
Dre. Emily Coffey ( Altering sleep and memory with sound )
Dr. Robert Zatorre ( The neuroscience of music and why we love it )
OHBM's many committees and Special Interest Groups
Community-led events at #OHBM2023
Read on to learn about upcoming committee and SIG events at OHBM 2023!
And don't forget to check out our latest Neuroscience podcast episode, where Peter Bandettini and Alfie Wearn talk about these events! You can find it at your favorite podcast service here and on YouTube here.
Rahul Gaurav & Naomi L. Gaggi
Looking at the past and future of functional connectivity

Dr. Biswal is well-known for his seminal work in functional connectivity and continues his research in brain connectivity and signal processing using MRI. He is also a familiar guest on the NeuroSalience Podcast, having been featured in Season 3, Episode 5 in conversation with his former labmate Dr. Peter Bandettini.
In this interview, Rahul Gaurav and Naomi L. Gaggi talked with Dr. Biswal as a keynote speaker for the upcoming 2023 Organization for Human Brain Mapping Conference in Montreal, Canada. They cover his academic journey, his research, and the potential future of resting state functional magnetic resonance imaging.
Lavinia Uscătescu, with editing by Xinhui Li
Capturing the complex activity of the social brain

In her 2023 OHBM keynote address, she will highlight some of her recent results developing extensive neuroimaging and neurostimulation protocols in a population of autistic children. Using transcranial magnetic stimulation (TMS), she stimulated structures of the social brain (i.e. the parts of the brain responsible for processing information related to social interactions and cues) and followed this up with both neuroimaging and clinical assessments.
In this interview, Dr. Xujun Duan discusses how she overcame the challenges of implementing a research protocol that would adequately capture the complex activity of the social brain, as well as the rewarding moments she enjoyed during this process. Additionally, she offers career advice for early stage researchers who plan on pursuing an academic path.
Elisa Guma and Kevin Sitek
Using a variety of methods to map circuits in the primate brain

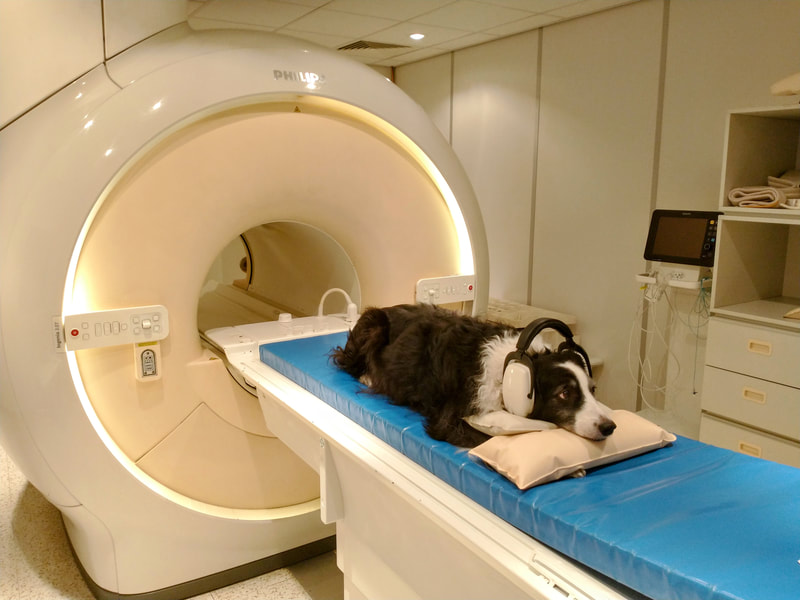
To address these questions, Dr. Minamimoto uses a range of methods including neuroimaging with functional MRI and PET as well as chemogenetic techniques such as Designer Receptors Activated by Designer Drugs (DREADDs), which are a class of proteins that allow scientists to control neural activity in awake, freely moving animals.
In this interview, Elisa Guma and Kevin Sitek talked with Dr. Minamimoto about his research program, the path he took to get there, and what we can expect from his 2023 Keynote address.
Read on to learn more!
Alfie Wearn and Faruk Gulban
Exploring quantitative MRI and 'in vivo histology'
Dr. Mezer’s lab is focused on mapping human brain structures during normal development and aging. In addition, it is focused on developing new approaches to characterize the structural changes associated with neurological disorders. Mezer’s main research tool is in vivo quantitative magnetic resonance imaging – qMRI. The Mezer lab is developing tools to biophysically explain the brain’s MRI signals at different levels and resolutions: from molecular local sources through cellular organization to the mapping of networks across the entire brain.
In this interview, we discuss the field of qMRI more broadly, touching upon the present and future interpretations of "in vivo histology." We also discuss Dr Mezer’s approach to mentorship, as well as the skills that would benefit future researchers in this field.
At OHBM 2023, Dr. Mezer will show us how combining multiple quantitative MRI measures can provide additional biological information about tissue composition and brain health.
You can find the video interview here and listen to the audio-only podcast version here (or on your podcast app of choice).
Johanna Bayer and LAVINIA CARMEN USCATESCU
Discussing deep brain stimulation and brain connectivity with Keynote presenter Andreas Horn

In this interview with Dr. Horn, we explore how deep brain stimulation can be used to better understand the human connectome, and how this work can be leveraged to improve patients’ lives. “In contrast to many other neuroimaging domains, there is a more or less direct translation [from Deep Brain Stimulation (DBS)] to clinical practice,” says Dr. Horn. For example, networks identified via DBS can be targeted with noninvasive stimulation methods such as multifocal transcranial direct current stimulation (tDCS) to improve conditions of patients with movement disorders like Parkinson's disease.
Dr. Horn also provides insight into ongoing discussions in the field on whether structural or functional measures provide better predictions for DBS outcomes. He explains why his lab has gradually shifted away from using patient-specific connectivity data to precise normative connectomes for determining which brain networks should be modulated for maximal effects.
In his keynote at OHBM 2023, Dr. Horn will give us a tour of his findings from years of work studying the effects of deep brain stimulation on the connectome across different disorders, ranging across neurological, neuropsychiatric, and psychiatric diseases. He will illustrate how his findings can be transferred across disorders to inform one another as well as how they can be further used to study neurocognitive effects and behaviors such as risk-taking and impulsivity.
You can find the video interview here and listen to the audio-only podcast version here (or on your podcast app of choice).
BLOG HOME
TUTORIALS
MEDIA
contributors
OHBM WEBSITE
Archives
January 2024
December 2023
November 2023
October 2023
September 2023
August 2023
July 2023
June 2023
May 2023
April 2023
March 2023
January 2023
December 2022
October 2022
September 2022
August 2022
July 2022
June 2022
May 2022
April 2022
March 2022
January 2022
December 2021
November 2021
October 2021
September 2021
August 2021
July 2021
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
December 2020
November 2020
October 2020
September 2020
June 2020
May 2020
April 2020
March 2020
February 2020
January 2020
December 2019
November 2019
October 2019
September 2019
August 2019
July 2019
June 2019
May 2019
April 2019
March 2019
February 2019
January 2019
December 2018
November 2018
October 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016













 RSS Feed
RSS Feed