Q&A with Dr Kihwan Han |
| Depression is a common psychiatric disorder amongst individuals with traumatic brain injury (TBI). Up to 77% of individuals with TBI have been found to experience depression. What can brain mapping tell us about depression after TBI? I met with Kihwan Han from the Center for Brain Health at the University of Texas at Dallas to talk about his recent research: an eight-week intervention that aimed at battling depression symptom severity in individuals with TBI. |
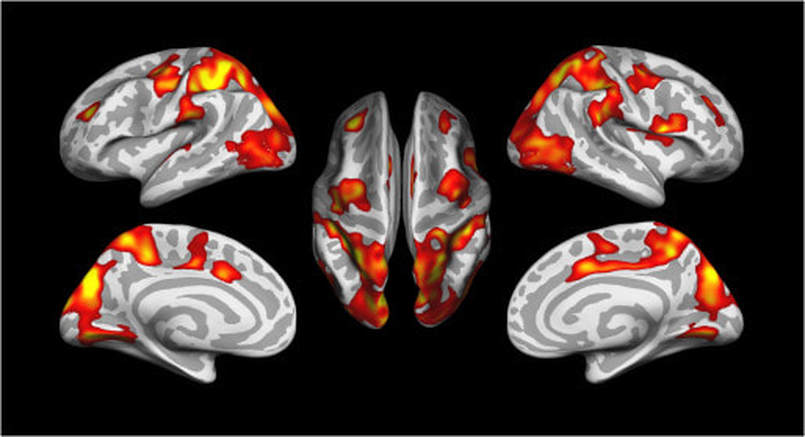
Kihwan Han (KH): In this study we investigated whether 8 weeks of cognitive training would reduce symptoms and severity of depression in individuals with chronic TBI. Indeed, we found reductions in depressive symptoms in individuals with mild-to-severe depressive symptoms compared to individuals with minimal depressive symptoms. Decreases in depression severity were also associated with improvements in self-reported post-traumatic stress disorder (PTSD) symptom severity, TBI symptom awareness and functional status. Further, reduced depressive symptoms were related to thickening of regional cortical gray matter and reductions in abnormal brain connectivity (Figure 2).
ED: How long have you been involved in TBI research and why are you interested in TBI?
KH: I started doing TBI research in 2011 as a post-doc in the neurology department at Washington University in St. Louis. The lab was exploring all aspects of TBI, including animal models.
ED: Do you think animal models of TBI, such as controlled cortical injury, can be informative?
KH: There is definitely strength in TBI animal research since a lot of variables can be controlled, with the ultimate goal of looking at what happens to the brain of humans when a TBI is sustained. The issue with animal research is that we are interested in how the brain functions after TBI but the animals and humans are different on the functional level. For example, the symptoms of TBI in humans are more complex.
ED: As you were just saying, TBI is a complex issue and usually researchers study aspects of different TBI severities. At OHBM, your presentation addressed not only TBI but also a complex mental disorder, specifically depression in individuals with TBI. What do you think is the value of studying psychiatric symptoms in clinical populations?
KH: TBI is a complex neurological event that leads to a variety of comorbidities. In military personnel with TBI, many researchers are looking at PTSD. But actually, depression is one of the most common psychiatric disorders in individuals with TBI. I think more and more researchers are starting to look at the different consequences of TBI, and depression should definitely be one of them, in my opinion.
ED: What do you think is the appeal of your work for broader audiences?
KH: I hope my research appeals to individuals with TBI and their loved ones who strive to get information about depression in TBI. My goal is for my research to give hope that there are rehabilitative solutions for individuals with TBI who also have depression. At the same time, I think my work should also appeal to scientists outside of the cognitive and clinical neuroscience fields, such as engineering. From the engineering point of view, TBI is a complex problem: one has to extract meaningful data from such a heterogeneous group of subjects. My background is actually in engineering and I started my postdoc with neurologists because they really needed help in analyzing the data, and were looking for someone who can bring a different perspective to the data. More people with diverse educational backgrounds are starting to do TBI research, so I think my research is appealing to people of different backgrounds.
ED: Can you briefly describe the next steps for your project?
KH: In the current project, we simply looked at the correlation between thickening of the gray matter and reduction of depressive symptomatology after an eight-week intervention. The next step will be to try and apply neuromodulation techniques to brain regions that were associated with a reduction of depressive symptomatology. Maybe neuromodulation can also lead to the reduction of depression symptoms.
Leave a Reply.
BLOG HOME
TUTORIALS
MEDIA
contributors
OHBM WEBSITE
Archives
January 2024
December 2023
November 2023
October 2023
September 2023
August 2023
July 2023
June 2023
May 2023
April 2023
March 2023
January 2023
December 2022
October 2022
September 2022
August 2022
July 2022
June 2022
May 2022
April 2022
March 2022
January 2022
December 2021
November 2021
October 2021
September 2021
August 2021
July 2021
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
December 2020
November 2020
October 2020
September 2020
June 2020
May 2020
April 2020
March 2020
February 2020
January 2020
December 2019
November 2019
October 2019
September 2019
August 2019
July 2019
June 2019
May 2019
April 2019
March 2019
February 2019
January 2019
December 2018
November 2018
October 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016

 RSS Feed
RSS Feed